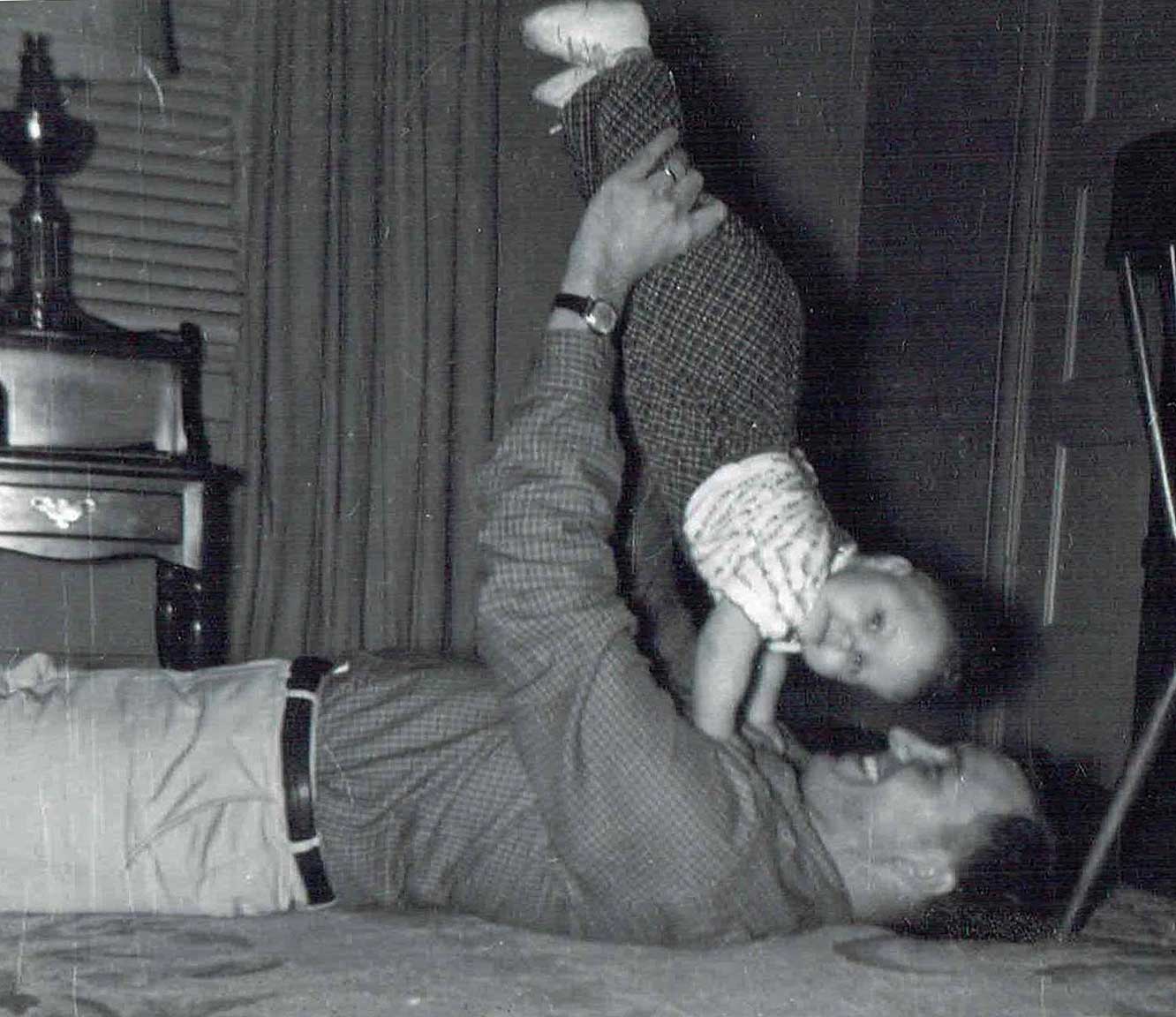
Pictured above with her father, Pamela Breyer, AIA is an architect with JSA Design in Portsmouth, NH. She specializes in environments for senior living.
Many baby-boomers help long-distance parents navigate health issues, housing changes and daily care. In my case, my father’s rapid health decline served as a fast-track introduction into the world of skilled nursing and hospice care, Oregon-style. A week in the hospital, a week in a (dad-detested) skilled nursing facility, five additional days in the hospital — suddenly it was time for hospice care and a suggestion to explore residential adult foster care. Adult foster care? Our family was hesitant — it seemed unlikely that adult foster care could compare favorably to the high-level care facilities that are available in medically sophisticated Portland, Oregon. My father required Level 3 care, difficult to locate in recommended facilities.
Working with placement team professionals, my family toured skilled nursing facilities with hospice care. We considered full-time home care to keep dad at home with our mother. These two options were not a good fit for our family.
Next we visited adult foster care homes. I had never heard of adult foster care until my father was in need, but hospital nurses strongly suggested we explore this unique west coast option. Adult foster homes are classified according to approved care levels and by how many Activities of Daily Living (ADL, basic self-care skills) the resident can independently perform. Several home visits later we found an adult foster home that seemed to fit the bill. My mother was comfortable with the home and care givers, and a room was available. Only one Level 3 patient per household is allowed in adult foster care, homes are allowed to care for a maximum of five people. Additional care required by patients (hospice, physical therapy or other special care) is provided by outside nurses with regular visits to these homes, and are contracted separately (usually covered by Medicaid or private health insurance) along with frequent spot checks by the Oregon DHS — Department of Human Services.
The foster care home we chose was newly licensed, with four resident rooms. It is managed by three sisters who have been in the senior care business their entire careers. A close family, their mother was their silent business partner and ran her own adult foster home close by. My father’s room was small with a set of French doors leading to a deck, while another door to the corridor allowed my father to hear household activity. The care-giving sisters were proactive in their approach to care — they offered my father anything they could dream up from the kitchen: lamb stew, cookies and special shakes they concocted. He was no longer eating, but he surprised us by taking bites of things, from popcorn to clementines. I kept a careful watch for his reactions but he never indicated that he wanted to go home, remaining sharp as a tack during our conversations. An outpatient hospice care company provided much of his daily medical care, counseled staff on the administration of pain medications, provided baths, and offered family support.
A shift from traditional institutional care
The passage of the HR3590 Health Care Reform Act will trigger a shift from traditional institutional care to a person-centered model of care. Many nationally respected models, such the Eden Alternative and Wellspring Innovative Solutions, already support person-centered care. This culture change extends to nursing home environments, encouraging individualized care delivery systems for better clinical success.
The Centers for Medicare & Medicaid Services (CMS) has proposed revisions updating the federal requirements that nursing homes must meet in order to participate in Medicare and Medicaid programs. These revised requirements directly affect the design of facilities with Medicare and Medicaid patients, prompting the reform of individualized care requirements. Practical implementation of the 483.75 Quality assurance and performance improvement regulations into a person-focused environment within a skilled nursing or standard nursing facility will require some innovative design solutions. The CMS recently partnered with the Pioneer Network to present a national symposium on culture change, “Creating the home in the nursing home,” beginning to bridge the gap between design changes and code issues.
It would be interesting if more states adopted this residential care option. While some families prefer more traditional care facilities, the personal relationship that develops between the caregiver, the patient and the family during this stressful time is very comforting. Although my mother feels lucky to have found this perfect fit for my father, she prefers a more private environment and has begun visiting assisted living communities for herself.
As an architect, my adult foster care experience was a fascinating eye opener in the quest to develop and provide attractive alternatives to traditional care facilities. For my family, adult foster care provided a warm and personal alternative to traditional end-of-life care. For my father, it meant a quiet and peaceful transition for his last few weeks, allowing him the dignity he deserved.
Read more about adult foster care and long-term care options:


